Kidney Conferences,Kidney Meetings,Kidney Events,Kidney Workshops,Kidney Symposiums,Kidney Conferences 2018,Kidney Conferences 2018,Kidney Conferences USA,Kidney Conferences Australia,Kidney Conferences UAE,Kidney Conferences Italy,Kidney Conferences Japan,Kidney Conferences South Korea,Kidney Conferences China,Kidney Conferences France,Kidney Conferences India,Kidney Conferences Poland,Kidney Conferences Spain,Kidney Conferences Germany,Kidney Conferences Brazil,Kidney Conferences Austria,Kidney Conferences Malaysia,Kidney Conferences Turkey,Kidney Conferences Finland,Kidney Conferences New Zealand,Kidney Conferences Ukraine,Kidney Conferences Philippines,Kidney Conferences UK,Kidney Conferences Canada,Kidney Conferences South Africa,Kidney Conferences Switzerland,Kidney Conferences Denmark,Kidney Conferences Mexico,Kidney Conferences Netherlands,Kidney Conferences Norway,Kidney Conferences Singapore,Kidney Conferences,Kidney Conferences, Renal Conferences, Kidney meetings, Kidney symposia, Kidney symposia, Renal symposia, Kidney Meetings
Kidney 2018 New York USA
Theme: Fostering kidney health across the Globe
Kidney 2018
On behalf of the Conference Series LLC Ltd and the scientific committee of Kidney 2018, we are pleased to welcome you to participate in the 3rd Annual Kidney Congress. The conference will be held from October 19 - 20, 2018 in New York City, NY, USA
|
Conference Name |
Place |
Date |
|
New York City, New York, USA |
Oct19-20, 2018 |
Both 3rd Annual Kidney Congress (October 19-20, 2018 in New York, USA) and 16th International Conference on Nephrology & Therapeutics (October 19-20, 2018 in New York, USA) are merged. In order to intensify the scientific arena, the organization has come to a decision of integrating both conferences.
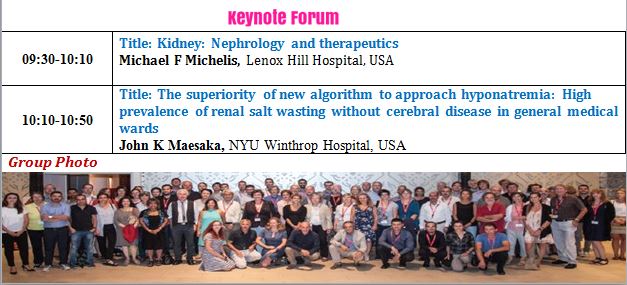
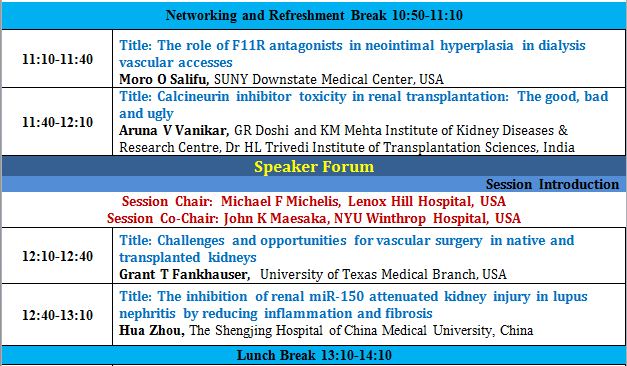
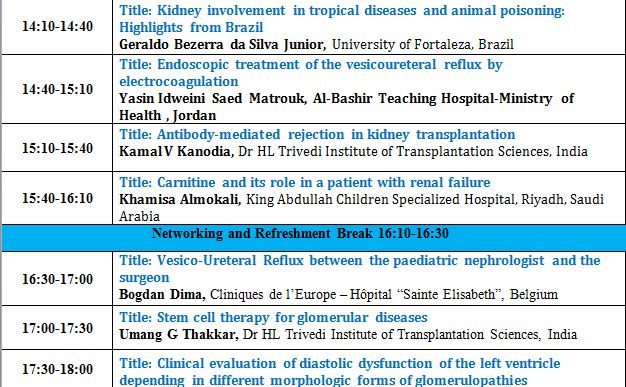
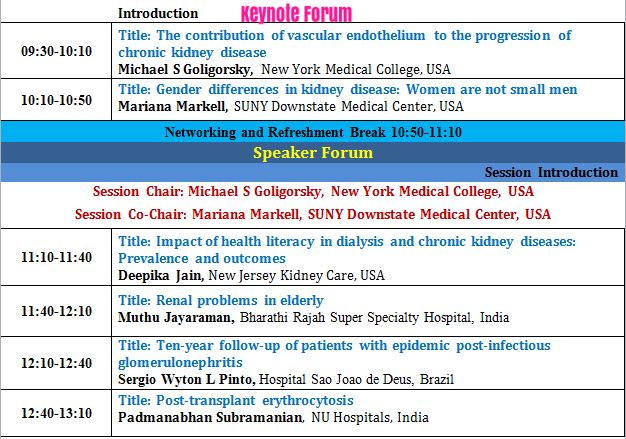
Program
Major scientific sessions:
| Kidney | Fluid, Electrolytes, Acid-Base Disorders |
| Acute Kidney Injury (AKI) | CKD -Mineral and Bone Disorders |
| Chronic Kidney Disease (CKD) | Kidney and Bladder stones |
| Dialysis and Renal Care | Urology/Urinary Tract Infections |
| Kidney Transplantation | Geriatric-Genetic Kidney Diseases |
| Pediatric Nephrology | Renal Nutrition |
| Kidney Cancer | Nephrology Nursing |
| Diabetic Kidney Disease | Diagnosis of Kidney Diseases |
| Cardiovascular Impacts of Kidney Disease | Renal Pathology-Immunology |
| Glomerular-Tubulointerstitial Disorders | Treatment, Drugs for Kidney Diseases |
Kidney 2018 Highlights includes:
CME (continues medical education)
CPD Continues professional development)
Keynote sessions by eminent and renowned researchers
Outstanding speaker sessions
International accredited certificates
All accepted abstracts for this Conference will be published in the respective International Journals
Abstracts will be published with DOI number by Cross Ref
Registrants will get 75% abatement on manuscript publication fees
Speaker and Abstract pages created in Google under your name will attract worldwide acknowledgment to your profile and research and it will be visible to 35K researchers across the globe
Special recognition for Young Researchers
One on One Meeting with top nephrologists
Symposia and Workshop sessions by distinguished nephrologists
Meetings with Top Industrial Representations
Special awards for Speakers and Poster Presentations
Group Registration benefits
Who Should Attend?
Nephrologists, Pediatric nephrologists, Urologists, Transplant Surgeons, Renal Dieticians, Renal Nurses, dialysis technicians, Radiologists, Cardiologists, Diabetologists, Family Physicians, Internists, Medical Students, Nurses, Pathologists, Medical Universities, Dialysis Centers, Dialysis equipment manufacturing companies, Pharmaceutical Companies, Associations and Societies
50+ speakers from all over the world
50+posterpresenations
10+exhibitors
150+ delegates
Hilton New York JFK Airport Hotel
Address: 144-02135th Avenue
Jamaica, New York 11436, USA
699 531
Track 1: Kidney
The paired retroperitoneal organs i.e. Kidneys lie behind the peritoneum between T12 to L3 vertebral bodies at an oblique angle. Kidneys have a fibrous capsule, which is covered by pararenal fat. Kidney itself can be divided into renal parenchyma, which consists of renal cortex and medulla, and renal sinus which contains renal pelvis, calyces, renal vessels, nerves, lymphatic and perirenal fat. Cortex and medulla are the two layers of renal parenchyma. Renal medulla consists of 10-14 renal pyramids and the renal cortex lies peripherally under the capsule, these are separated from each other by renal cortex named renal columns. Kidneys perform major functions, which include ultrafiltration and excretion of metabolic waste products like urea and ammonium, maintenance of electrolytes balance, fluid and acid-base balance; and also for red blood cell production. They are also important agents behind regulation of blood pressure through renin-angiotensin-aldosterone system, by controlling reabsorption of water they maintain intravascular circulatory volume.
This category includes the following sub topics: kidney failure, nephrotoxicity, Iga nephropathy, alport syndrome, minimal change disease, new kidney diseases, kidney and anaemia, inherited kidney diseases, medullary sponge kidney, advances in nephrology, renal histopathology, kidney stones, nephronophthisis, nephroptosis, clinical nephrology-general aspects, infection and renal disease.
Track 2: Acute Kidney Injury (AKI)
Acute renal failure (ARF), previously called acute kidney injury (AKI), is a sudden and unexpected loss of kidney function which may develop within a week. Acute renal failure (formerly known as acute kidney injury) is a disease distinguished by the acute loss of the kidney's eliminatory function and is commonly diagnosed through the accumulation of urea and creatinine or reduced urine output, or both. Acute kidney injury may lead to a number of kidney problems, including high potassium levels, metabolic acidosis, changes in body fluid balance, uremia, and also affects other body system ultimately leading to death. Patients who have experienced acute kidney injury may have high potential of suffering from chronic kidney disease in their future. Controlling measures include treatment of the root cause and supportive care, such as kidney transplantation.
This session includes Acute Kidney Injury–Experimental Models, Clinical Studies including Toxic Nephropathy, Biomarkers for Acute Kidney Injury, Acute Renal Failure–Clinical, Acute Kidney Injury-Onco-Nephrology (Diseases), Acute Kidney Injury–Onco-Nephrology (Drugs), Acute Kidney Injury–Pregnancy (Pre-Eclampsia, TMA, HELLP, Other Causes), Acute Kidney Injury–Update on CRRT, SLED, Extracorporeal Therapies - Intoxications, Overdoses, Liver Failure, etc.
Track 3: Chronic Kidney Disease (CKD)
End-stage renal disease also termed as chronic kidney diseases (CKD) comprise of conditions that damage kidneys and impair their ability to maintain hygiene by abnormality in functions. Such conditions make kidney disease worse; wastes can accumulate to high levels in patient blood and make them feel sick. Issues like anaemia, high blood pressure, weak bones, nerve damage and poor nutritional health. Also, kidney disease elevates the risk of having coronary disease and heart problems. These problems may occur gradually over a long period of time. Diabetes and high blood pressure are the two main causes of chronic kidney disease.
It covers CKD: Fibrosis and Extracellular Matrix CKD, CKD Mineral and Bone Disorder, Acid Base and Electrolyte Abnormalities, Cardiovascular Complications of CKD 3-5, Chronic Kidney Disease Diagnosis, Classification and Progression, Epidemiology, Outcomes and Health Service Research in CKD, Bone and Mineral Metabolism, Anaemia (CKD 3-5), Nutrition (CKD 3-5), Infection (CKD 3-5), Chronic Kidney Disease–Mesoamerican Nephropathy, Chronic Kidney Disease–Diseases and Drugs.
Track 4: Dialysis and Renal Care
The most common form of kidney replacement therapy is dialysis, is a way of cleaning the blood with artificial kidneys. There are following types of dialysis:
- Haemodialysis
- Peritoneal dialysis.
Haemodialysis is required with the patients of renal failure. In this process of haemodialysis, an artificial kidney purifies blood. We should make an "access," usually in the forearm from where blood can easily be taken from the body and sent to the artificial kidney for purification. The access collects blood from the patient’s body and then the blood undergoes purification in those artificial kidneys and is again injected back after purification into the patient’s body.
In peritoneal dialysis no artificial kidney is used. The peritoneum (lining inside your abdomen) is used as a filter instead of artificial kidney. Peritoneal dialysis is of two types they are continuous cycling peritoneal dialysis and continuous ambulatory peritoneal dialysis. Peritoneal dialysis is used in patients having kidney failure.
In this track we discuss Haemodialysis, Peritoneal Dialysis, Home Dialysis, Extracorporeal Dialysis: Techniques and Adequacy, Vascular Access in Dialysis, Complications of Dialysis, Epidemiology, Outcomes and Health Services Research in Dialysis, Transplantation: Basic Science and Immune Tolerance, Clinical Studies in Renal Transplantation, Cardiovascular Complications of CKD 5D, Bone and Mineral Metabolism (CKD 5D), Conservative Management of Advanced CKD (vs. Dialysis), Palliative Care for CKD/ESRD, Dialysis Solutions, Infection, Membrane Biology, Membrane Function, Quality of Life in Dialysis.
Track 5: Kidney Transplantation
Kidney Transplantation is the mechanism of surgical implantation of a kidney from the external which assumes control over the function of purification of blood by performing surgery in patients with kidney failure. It is delegated either by living contributor transplantation or perished benefactor transplantation on the wellspring of organ of the giver. Kidney transplantation is the decision of treatment when kidneys fall flat alongside haemodialysis and peritoneal dialysis. kidney transplants are categorized into two types: those that are carried out from contribution by living contributors and those which occur from inconsequential givers (non-living donors). Kidney transplant would be possible for patients who: could withstand the impacts of surgery, the effects of immunosuppressant pharmaceuticals,, medicines after transplantation. It is possible to give a kidney while you are alive and lead a completely normal healthy life on the grounds that only one kidney is needed to survive.
Under this we have the following topics: Advances in Kidney Transplantation, Transplantation Techniques, Pediatric Renal Transplantation, Dual Kidney Transplantation, Pregnancy after Transplantation, Post-Transplant Complications, Acute Renal Allograft Rejection, Stem Cell Transplantation, Pediatric Nephrology, Screening Tests, Transplantation – Epidemiology, Transplantation – Immunosuppression, Transplantation – Outcomes, Transplantation – Surgery.
Track 6: Pediatric Nephrology
Pediatric Nephrology is a specialization in the diagnosis and management of children with different types of acute and chronic kidney-related diseases. The division assesses and treats hypertension, proteinuria, hematuria, renal tubular acidosis, glomerulonephritis, nephrolithiasisand kidney disorders. Various kidney diseases like pediatric nephritisare clinically and hereditarily heterogeneous substance portrayed by backsliding, and interminable course with noteworthy dreariness and mortality coming about because of intricacies of the sickness itself, and its treatment.
This session covers Comprehensive Pediatric Nephrology, Clinical Pediatric Nephrology, Pediatric Renal Failure, Diagnostic Techniques, Advanced Therapies, Pediatric Renal Transplantation, Advances in Kidney Operation, Pediatric Kidney Dialysis, Pediatric Kidney Care and Pediatric Kidney Failure Diet.
Track 7: Kidney Cancer
Kidney cancer (also called renal adenocarcinoma or renal cell cancer) is a disease in which cancer cells are found within the lining of tubules in the kidney. We have two kidneys, behind the peritoneum one on each side of the spinal cord.. Small tubules in the kidneys purify the blood. Unabsorbed products are formed as urine. The urine then passes in to the urinary bladder through long tubes called ureter one coming from each kidney and joining the bladder. The urine is stored in bladder until it leaves the body through urethra. Kidney cancer perhaps remains clinically occult for most of its course. Immunomodulatory agents and targeted therapy are the standard care measures in metastatic disease patients. The most common malignant disease affecting kidney is kidney cancer. One of the most common causes for kidney cancer is smoking.
This track includes renal cell carcinoma, Types of renal cell carcinoma, renal cell carcinoma risk factors, Pathophysiology, Treatment and Outcomes, Chemotherapy, Immunotherapy, Targeted Therapy.
Track 8: Diabetic Kidney Disease
The diabetic kidney disease sometimes also called as diabetic nephropathy is a kidney related complication which may occur in people with diabetes mellitus. In diabetic nephropathy, filters of the kidneys and glomeruli become damaged. In this condition the kidneys leak abnormal quantity of protein from blood into the urine. If anyone has diabetes, the blood glucose, or blood sugar levels are very high. For prolonged period, this can damage the kidneys. The role of kidney is to clean your blood. In case they are damaged, waste and fluids accumulate in your blood with out of leaving from your body. If the kidney damage by diabetes is called diabetic nephropathy. Usually it starts long before you have notice symptoms. The beginning sign of it is small quantity of protein in urine. By urine test we can detect diabetic nephropathy or blood test can also determine the functioning of kidneys.
Diabetic kidney disease session covers diabetic nephropathy, diabetes mellitus (clinical), diabetic nephropathy–biomarkers of disease, intensive management of blood glucose, genetics of kidney disease–diabetic kidney disease, hypertension-clinical and experimental models, renal haemodynamics and vascular physiology.
Track 9: Cardiovascular Impacts of Kidney Diseases
Kidney diseases may also lead to heart disease or coronary illness because of which more than 20 million people die in the U.S.. Chronic kidney disease induces the risk of death from cardiovascular disease. Coronary disease results in more than half of all the deaths among individuals with CKD (Chronic kidney diseases). Indeed, even early stage of renal ailment puts a man in the risk zone of heart ailments and heart attacks and also heart disease-related death. Kidney dialysis patients who also have cardiovascular disease are more prone to death at about 10 to 30 times than in case of general cardiovascular patients. Diabetes and hypertension are two major risk factors for heart disease and chronic kidney disease. Kidney disease (acute kidney disease or chronic kidney disease) can induce the danger of cardiovascular illness, even with hypertension, high cholesterol and concurrent diabetes. Recent researches show that kidney diseases (renal diseases) induce heart disease, even before the kidneys are harmed to the point of requiring dialysis or transplantation
The session includes Cardiorenal syndrome, Effects of Cardiovascular Diseases on the Kidney, Effects of the Kidney on the Cardiovascular System, Diseases Affecting both Organs, Modification of Cardiac Drugs in Renal Disease, Hypertension, Kidney and Vascular Diseases, Etiology and classification, Essential hypertension, Hypophosphatemia, Hyperuricemia, Hyperkalemia, Hypertension, CKD and Diabetes, Reno vascular hypertension, Anti hypersensitive therapy, Recent Advances in Glomerular Disorders and Hypertension, Anaemia and Erythropoietin, Renal Osteodystrophy.
Track 10: Glomerular-Tubulointerstitial Disorders
Abnormal glomerular function may lead to damage of glomerulus components such as capillary endothelium, mesangium and epithelial basement membrane. In renal biopsy we can see cellular and structural pattern of glomeruli injury by using electron microscopy. As per the time of examination and the intensity of the lesions, in vascular diseases and glomerular ones we can identify tubular damage in glomerulus, interstitial inflammation, tubular atrophy, fibrosis or edema. Tubular or acute interstitial damage may lead to acute kidney failure, and prolonged changes are a best investigation parameter for irreversible lesions and then they are great anticipatory variables in vascular /glomerular diseases.
This session includes Glomerulonephritis, Glomerulopathy, Acute Pyelonephritis, Chronic Pyelonephritis, Acute Infectious Tubulointerstitial Nephritis (Tin), Tin Associated with Systemic Infection, Chronic Infectious Tin (Chronic Pyelonephritis) and Specific Renal Infections Xanthogranulomatous Pyelonephritis, Acute Interstitial Nephritis Associated to Drugs, Acute Tubular Necrosis and Other Tubular Changes.
Track 11: Fluid, Electrolytes, and Acid-Base
The renal system maintain homeostasis in the body by avoiding significant modifications in the balance of fluid electrolyte or acid–base parity until the Glomerular filtration rates are reduced down to below 25 ml/min because of a series of versatile changes, both renal and extra-renal. With a dynamic decrease in renal capacity, these components are overpowered by bringing about unsettling influences in water digestion system adding to hypernatremia and hypernatremia. The modified control of sodium transport causes irritated volume status including volume over-burden and exhaustion. The rate of Hyperkalemia and metabolic acidosis is more incessant in Chronic Kidney Disease (CKD) with GFR below 10 ml/min. This session covers Disorders of Plasma Osmolality, Electrolyte Disorders in Diabetes Mellitus, Hydration in Kidney Disease Prevention, Disturbances of Plasma Sodium Concentration, Disturbances of Plasma Potassium Concentration, Disturbances of Plasma Calcium Concentration, Physiology of Acid-Base System, Metabolic Acidosis, Respiratory Acidosis, Metabolic Alkalosis and Respiratory Alkalosis.
Track 12: CKD -Mineral and Bone Disorders
The mineral and bone metabolism disorders (MBD) are common in patients with chronic kidney disease. Conventionally, these disorders are collectively termed as renal osteodystrophy. We can see mineral and bone disorders in patients with chronic kidney diseases, calcium and phosphorus levels in patient’s blood to be out of balance due to imbalance of hormones. This leads to kidney failure and dialysis.
The kidneys assume an essential part in maintaining sound bone mass and structure by adjusting phosphorus and calcium levels in the blood. Healthy kidneys actuate a type of vitamin D which a man expends in sustenance, transforming it into calcitriol, the dynamic variety of the vitamin. Calcitriol helps the kidney to maintain blood calcium levels and advances the arrangement of bone. The kidneys likewise expel additional phosphorus, adjusting levels of phosphorus and calcium in the blood. It also helps to maintain the best possible level of phosphorus in the blood keeping the bones healthy.
CKD -Mineral and Bone Disorders covers Mineral and bone disorder in chronic kidney disease, mineral and bone disorder in children with chronic kidney disease, cardiovascular calcification, treatment with active forms of vitamin D.
Track 13: Kidney and Bladder stones
Kidney or bladder stones are the crystals of calcium oxalate and uric acid. If a kidney stone obstructs the urethra or the ureter, it results in haematuria (blood in the urine), constant and severe pain in the back or side, fever, vomiting, or chills. Nephrolithiasis (Kidney stones): Minerals in urine form stones, which may generate into a size big enough to block the flow of urine. Most kidney stones pass through urine on their own but some kidney stones are too large and they cannot pass hence should be treated.
Bladder stones are hard masses of minerals in the urinary bladder. Bladder stones create when urine in the bladder becomes more concentrated, resulting in the minerals to take up shapes. Concentrated, stagnant urine is the regular after-effect of not having the capacity to totally exhaust the bladder. On the off chance that bladder stones are sufficiently small, they can go all alone with no detectable indications. In any case, once they get bigger, bladder stones can bring about incessant inclinations to urinate, excruciating or troublesome urination and haematuria.
This session includes Kidney stones, bladder stones, treatment, surgery, artificial kidney, diet for stones, transplant research.
Track 14: Urology/Urinary Tract Infections
This category includes diseases of the urinary system, prostate gland including the kidneys and bladder. The bladder or urethra usually is affected in any urinary tract infections, yet more genuine and serious infections include the kidney. A bladder disease may bring about pelvic torment, excessive inclination to urinate, torment with urination process and blood in the urine. Renal infection may bring about back agony, sickness, heaving and fever.
Urology/Urinary Tract Infections cover Urethritis, Pyelonephritis, Cancers of the Kidney and Genitourinary Tract, Diagnosis of Kidney and Urinary Tract Disorders, Disorders of Kidney Tubules, Disorders of Urination, Obstruction of the Urinary Tract, Stones in the Urinary Tract.
Track 15: Geriatric-Genetic Kidney Diseases
Some renal diseases like Polycystic Kidney Disease (PKD) are result of hereditary factors. In polycystic kidney disease, number of cysts develops in the kidneys. These cysts gradually replace the mass of kidney impairing kidney function and leading to renal failure.
Geriatric nephrology is a developing subspecialty for older patients. Patients having a longer life span may be prone to infections which quicken perpetual kidney diseases, and remain undetected until patients are defied with the sudden requirement for dialysis. Renal cystic illness includes an extensive variety of sickness elements. They can be named either (1) inherited or obtained or (2) systemic or renal limited illnesses that have the normal element of numerous renal pimples. Every malady substance contrasts in its presentation, anticipation, and administration. Renal sores are smooth-walled, liquid filled round structures framed by central out pouching of renal tubules. In any case, huge steps have been taken of late. For autosomal predominant and autosomal passive polycystic kidney sicknesses (ADPKD and ARPKD), a photo is beginning to rise. Waste products in the essential ciliary detecting systems, intracellular calcium control, and cell cyclic AMP (cAMP) aggregation, all appear to assume a part in the modified cell phenotype and capacities.
Geriatric-Genetic Kidney Diseases include the following topics: Inherited Kidney Diseases, Renal Cystic Diseases, Polycystic Kidney Disease (PKD), Kidney Disease in Elderly Diabetic Patients, Drug Dosing and Renal Toxicity in the Elderly Patient, Glomerular Disease in the Elderly, Hypertension, Chronic Kidney Disease, and the Elderly, Cardiovascular Disease in the Elderly with Kidney Disease, Vascular Disease in the Elderly.
Track 16: Renal Nutrition
Syndrome of protein-energy wasting consists of nutritional and metabolic abnormalities seen in chronic kidney disease. It is very essential to maintain maintain a healthy lifestyle for people with renal disorders, especially if that is accompanied by high blood pressure, diabetes, or both. Control and maintainence of normal blood glucose levels can help to prevent or postpone diabetic complications, including kidney diseases. What we eat and drink may help slow down kidney disease. Dieticians could guide patients on how to organise a diet that is safer for the kidneys by considering the concentrations of protein, potassium, phosphorus, sodium, and how to read food leaflets and labels.
Track 17: Nephrology Nursing
Nephrology nurses are engaged in caring for patients of all age groups who are experiencing, or are at risk of kidney disease.
Nephrology nursing involves both preventing disease and assessing the health needs of patients and their families. Care spans the life cycle and involves patients who are experiencing the real or threatened impact of acute or chronic kidney disease; therefore nephrology nurses must be well-educated, highly skilled, and motivated. These nurses also deal with every organ system in the body, bringing about a holistic approach in patient care which is both challenging and rewarding.
Driven by technological and educational advances, nephrology nursing continues to be a dynamic field with a wide variety of career opportunities for nurses at all levels.
Nephrology Nursing session covers Nephrology Nursing, Dialysis nursing, Cannulation, Home dialysis nursing, Kidney care nursing, Health Care and Management, Kidney Cancer & Tumor Nursing Pediatric Nursing, Surgical Nursing, Rehabilitation Nursing, Clinical Nursing, Nursing education, Critical care and Emergency Nursing, Nursing Management, Nurse Practitioner Updates.
Track 18: Diagnosis of Kidney Diseases
Healthy kidneys remove wastes and excess fluid from the blood. Blood and urine tests show how well the kidneys are functioning and how quickly body wastes are being eliminated. Urine tests can also detect whether the kidneys are leaking abnormal amounts of protein, a sign of kidney damage. Imaging tests use sound waves to get an image of the kidneys. It may be used to diagnose any form of abnormalities in size or position of the kidneys or for obstructions such as stones or tumors.
Track 19: Renal Pathology-Immunology
The kidneys are often targeted by pathogenic immune responses against renal auto antigens or by local manifestations of systemic autoimmunity. For the diagnosis renal pathologists use special tests and electron microscopes to detect the cells involved in diseases affecting the kidneys.
Kidney biopsies permit us to analyze renal disorders; review anticipations; help in resolving a precise restorative approach; and screen ailment movement in both local and allograft transplant kidneys. To maximally abuse renal biopsy examples, a blend of light, immunofluorescence and electron microscopy is used. Each microscopy requires distinctive strategies for fixation and preparing, so each renal biopsy centres are commonly separated into three sections. Contingent upon the length of the biopsy centre or suspected illness process; in any case, the strategy for partitioning the biopsy centre may be altered.
Track 20: Drugs for Kidney Diseases
Nephrologists will work to slow or control the reason behind kidney diseases. Depending on the root cause, some types of kidney disease can be treated. Frequently, though, chronic kidney disease has no prevention. In the event that the kidneys turn out to be seriously harmed, the patient may require treatment for end-stage kidney diseases. By then, dialysis or a kidney transplant is required. Since no particular in option and Ayurveda prescription for kidney can treat kidney disappointment successfully, the best technique is to join them. Immunotherapy, is an extraordinary leap forward in treating end-stage kidney sickness, and is an excellent and versatile blend of cutting edge western restorative advances and customary home grown drugs.
3rd Annual Kidney Congress
Welcome:
Conference Series LLC Ltd takes the pleasure of inviting people from all over the world to take part in the 3rd Annual Kidney Congress which is going to be held in New York, USA during October 19-20, 2018.The conference aims at bringing people from all over the world under one platform for timely exchange of innovative ideas in the field of Nephrology and renal care. The conference includes prompt keynote presentations, Oral talks, Poster presentations and Exhibitions conducted by eminent speakers and scholars bearing reputed degrees in the field of Nephrology and related science.
Kidney 2018 conference deals with all the therapeutic aspects and remedial technologies In the field of renal science providing a roof for all the people, nephrologists and kidney specialists from leading universities and research institutions to foster their ideas and bring collaboration and advancements in the field of nephrology across the globe.
Scope and Importance
Kidney 2018 will cover the latest advances in the field of hemodialysis, going from uremic toxins, Kidney diseases, hemodiafiltration, advancements in hemodialysis, dialysis in intense kidney damage, and complexities of kidney damage including mineral bone ailment, iron deficiency, and cardiovascular infections.
This event was originally conducting for the Public healthcare team, including nephrologists, clinical specialists, general surgeons, kidney transplant surgeons, surgical and nephrology nurses, dialysis technicians, social workers and renal nutritionists. It was also designed to be of interest to other health care professionals and primary care physicians.
List of Societies Associated with Nephrology Research around the Globe:
African Association of Nephrology (AFRAN), Congolese Society of Nephrology (CSN), Egyptian Society of Nephrology, Kenya Renal Association, Moroccan Society of Nephrology, Nephrology Society of Tanzania, Nigerian Association of Nephrology, Senegalese Society of Nephrology, South African Renal Society, Sudanese Society of Nephrology, Tunisian Society of Nephrology, Albanian Society of Nephrology, Association for nephrology, dialysis and transplantation of Bosnia and Herzegovina, Bulgarian Society of Nephrology, Croatian Society of Nephrology, Dialysis & Transplantation, Estonian Society of Nephrology, Hungarian Society of Nephrology, Latvian Association of Nephrology, Macedonian Soc. of Nephrology, Dialysis, Transplantation and Artificial Organs , Moldavian Society of Nephrology, Montenegrin Association of Nephrologists, Polish Society of Nephrology, Romanian Society of Nephrology, Association of Cardionephrology of Serbia, Slovenian Society of Nephrolog, Turkish Society of Nephrology, Argentina Society of Nephrology, Bolivian Society of Nephrology, Brazilian Society of Nephrology, Chile Society of Nephrology, Colombian Society of Nephrology, Costa Rican Society of Nephrology, Cuban Society of Nephrology, Ecuadorian Society of Nephrology, Association of Nephrology and Hypertension of El Salvador, Guatemalan Society of Nephrology, Latin-American Society of Nephrology and Hypertension, Mexican College of Nephrologists, Mexican Institute for Nephrologycal Research, Nicaraguan Association of Nephrology, Panamanian Society of Nephrology, Paraguayan Society of Nephrology, Peruvian Society of Nephrology, Puerto Rican Society of Nephrology and Hypertension, Uruguayan Society of Nephrology, Venezuelan Society of Nephrology, Arab Society of Nephrology & Renal Transplantation, Emirates Medical Association Nephrology Society, Iranian Society of Nephrology, Jordan Society of Nephrology and Renal Transplantation, Kuwait Nephrology Association, Lebanese Society of Nephrology & Hypertension, Saudi Society of Nephrology, Syrian Society of Nephrology & Transplantation, Yemen Society for Nephrology and Transplantation, Dialysis, Nephrology and Kidney Transplantation Union of Georgia, Society of Nephrologists, Dialysis and Transplant Physicians of Kazakhstan, Russian Dialysis Society, Asian Pacific Society of Nephrology, Chinese Society of Nephrology, Hong Kong Society of Nephrology, Japanese Society of Nephrology, Korean Society of Nephrology, Mongolian Society of Nephrology and Urology, Taiwan Society of Nephrology, American Society of Nephrology, Canadian Society of Nephrology, Australian and New Zealand Society Of Nephrology, Cambodian Association of Nephrology, Indonesian Society of Nephrology, Malaysian Society of Nephrology, Myanmar NephroUro Society, Nephrology Society of Thailand, Philippine Society of Nephrology, Singapore Society of Nephrology, Bangladesh Renal Association, Indian Society of Nephrology, Nepalese Society of Nephrology, Pakistan Society of Nephrology and Urology, Sri Lanka Society of Nephrology, Austrian Society of Nephrology, Belgian-Dutch Speaking Society of Nephrology, British Association of Pediatric Nephrology, Danish Society of Nephrology, Dutch Federation of Nephrology, French Society of Nephrology, German Society of Nephrology, Hellenic Society of Nephrology, Irish Kidney Association, Irish Nephrology Society , Israel Society of Nephrology and Hypertension, Italian Society of nephrology, Norwegian Society of Nephrology, Portuguese Society of Nephrology, Renal Association, Spanish Society of Nephrology/Fundacion Senefro, Swedish Society of Nephrology, Swiss Society of Nephrology
Conferences related with Nephrology Worldwide:
Annual Dialysis Conference, World Nephrology Congress (WCN), Kidney Week, International Conference on Nephrology, ISN World Congress of Nephrology, 20th International Conference on Dialysis, 37th Annual Advanced Nephrology: Nephrology for the Consultant, Glomerular Disease, Updates 2018 - 7th Annual, The 7th Annual Glomerular Conference, Cutting Edge of Transplantation - Transplant Summit 2018, 16th Annual Mayo Clinic Update in Nephrology and Transplantation 2018, 23rd International Conference on Advances in Critical Care Nephrology (AKI & CRRT 2018), Nephrology 2018, Update in Nephrology and Hypertension 2018, American Transplant Congress (ATC), 17th Congress of the International Society of Peritoneal Dialysis (ISPD 2018), 2017 Onco-Nephrology Symposium, American Urological Association (AUA) 2018 Annual Meeting, 18th Annual Meeting of the Society of Urologic Oncology, EDGE Endourology and Enucleation Symposium 2018, National Kidney Foundation Spring Clinical Meeting (SCM 2018), National Family Medicine Board Review 2018, 16th Annual Update in Nephrology and Kidney Transplantation 2018, Controversies in Dialysis Access (CiDA) 2018, Kidney Cancer Association (KCA) Patient and Survivor Conference 2017, Continuous Renal Replacement Therapy (CRRT) University Pediatric Centered Care Conference 2017, Advanced Practices in Acute Kidney Injury (APAKI) 2018, American Society of Diagnostic and Interventional Nephrology (ASDIN) 14th Annual Scientific Meeting, Volhard-Fahr Nephropathy Course 2018, International Society of Nephrology (ISN) Frontiers Symposium 2018, Renal Physicians Association (RPA) Annual Meeting 2018, Harvard Medical School (HMS) Nephrology 2018, American Nephrology Nurses Association (ANNA) 49th National Symposium, Update on Chronic Kidney Disease 2018, Nephrology Update 2018, 12th International Podocyte (IPC) Conference, Updates in Kidney Transplant and Donation 2018, 41st Annual Postgraduate Medicine Course: The Columbia Renal Biopsy Course, Nephrology Nursing Practice, Management, & Leadership Conference, National Renal Administrators Association (NRAA) Annual Fall Conference 2018, Canadian Society of Nephrology (CSN) Conference in America 2018, Florida Society of Nephrology (FSN) Annual Meeting 2019, American Nephrology Nurses Association (ANNA) 50th National Symposium, Polycystic Kidney Disease, Treating to Target in Patients with Gout and Chronic Kidney Disease: A Patient Simulation, Continuous Renal Replacement Therapy: Case Vignettes, Fabry Disease: When to Treat, Kidney and Kidney-Pancreas Transplantation: Evaluation and Management, Virtual Symposium: Evolving Therapeutic Paradigms for the Management of Hyperkalemia, Pediatric Hypertension - UC Davis Pediatric Nephrology series, 2017 Memorial Sloan Kettering Cancer Center Onco-Nephrology Symposium, Inaugural Jefferson Urology Symposium: Innovations in the Endoscopic Use of the Holmium Laser, Kidney Conferences, Nephrology Conferences, Renal Conferences, Kidney Transplantation Conferences, Dialysis Conferences, Kidney Meeting, Kidney Event, Kidney Symposiums, Kidney Conference, Nephrology Conference, Renal Conference, The National Kidney Foundation, Kidney Transplantation Conference, Kidney Meetings, Kidney Events, Kidney Symposium, Kidney Expo, Dialysis Conference, Kidney Summit, Kidney Workshop, Global Kidney conference, International Kidney Conference, Kidney Week, Annual Kidney Conference, Kidney Conference in USA, Nephro Conference, World Nephrology Conference, Nephrologists Conference, Euro Nephrology Conference, Society Conference, National Kidney foundation Conference, The Kidney Summit
Hospitals Associated with Nephrology around the world:
Mayo Clinic, Cleveland Clinic, Johns Hopkins Hospital, New York-Presbyterian Hospital, UCSF Medical Center, Ronald Reagan UCLA Medical Center, Hospitals of the University of Pennsylvania-Penn Presbyterian, Massachusetts General Hospital, Barnes-Jewish Hospital, Mount Sinai Hospital, Albany Medical Center, Albert Einstein Medical Center, Allegheny General Hospital, Baylor College of Medicine, Baylor University Medical Center, Beth Israel Deaconess Medical Center, Boston Medical Center, Brigham and Women's Hospital, Brookdale University Hospital and Medical Center, Rhode Island Hospital, University Hospitals Case Medical Center, Cedars-Sinai Medical Center, Cleveland Clinic Florida, Cleveland Clinic Foundation, Cooper University Hospital , Dartmouth-Hitchcock Medical Center, Wayne State University/Harper Hospital , Hahnemann University Hospital, Duke Nephrology, Emory University School of Medicine, Geisinger Health System, George Washington University Medical Center, Georgetown University Hospital , Harlem Hospital Center, Hennepin County Medical Center, Henry Ford Hospital, Lenox Hill Hospital, Staten Island University, Mount Sinai Beth Israel Hospital, Mount Sinai School of Medicine, Mount Sinai Medical Center, Mount Sinai St. Luke's Hospital, Indiana University School of Medicine/Nephrology, University of Miami School of Medicine, Jacobi Medical Center, Johns Hopkins University School of Medicine, Kaiser Foundation Hospital, Lehigh Valley Health Network, Loma Linda University, Los Angeles County-Harbor- UCLA Medical Center, Louisiana State University Health Sciences Center, Louisiana State University Medical Center, Loyola University Medical Center, Maimonides Medical Center, Lankenau Medical Center, Maine Medical Center, Marshall University School of Medicine, Mayo Clinic Hospital College of Medicine, Mayo Clinic, Mayo School of Graduate Medical Education, Northwestern University, Feinberg School of Medicine, Georgia Regents University, Medical College of Wisconsin, Medical University of South Carolina, Methodist Health System Dallas, Methodist Hospital (Houston), Albert Einstein College of Medicine, Nassau University Medical Center, Walter Reed National Military Medical Center, Metropolitan Hospital Center, New York Medical College at Westchester Medical Center, New York Presbyterian Hospital, New York University Medical Center, New York Presbyterian /Queens, Newark Beth Israel Medical Center, Ochsner Clinic Foundation, Ohio State University Hospital, Olive View-UCLA Medical Center, Oregon Health & Science University, Penn State Milton S Hershey Medical Center, Rish University Medical Center, Rutgers New Jersey Medical School, Rutgers Robert Wood Johnson Med School, Christiana Care Health System, Thomas Jefferson University Hospital, St John Hospital and Medical Center, St Louis University School of Medicine, Stanford University, SUNY at Stony Brook Health Science Center, SUNY Downstate Medical Center, SUNYUpstate Medical University at Syracuse, Temple University Hospital, Scott & White Memorial Hospital, Texas Tech Univ Health,Sciences Center at Lubbock, Texas Tech University Hlth Sci, Ctr Paul L. Foster Sch of Med, Tufts Medical Center, Tulane University School of Medicine, UCLA School of Medicine, Baystate Medical Center, Veterans Administration WNY, Healthcare System, University of Alabama at Birmingham, University of Arizona, University of Arkansas for Medical Sciences, University of California (Davis) Medical Center, University of California Irvine Medical Center, UCSD Medical Center, Hillcrest University of California (San Francisco), University of Chicago Hospitals and Clinics, University of Cincinnati Medical Center, Division of Renal Diseases and Hypertension, University of Connecticut Health Center, University of Florida College of Medicine Jacksonv, University of Florida Medical Center, University of Illinois Hospital, University of Iowa Hospitals and Clinics, University of Kansas Medical Center, University of Kentucky Medical Center, Univeristy of Louisville Nephrology, University of Maryland Medical System, University of Massachusetts, Medical School, University of Michigan Hospitals, University of Minnesota Hospital & Clinic, University of Mississippi Medical Center, University of Missouri Health Sciences Center, University of Nebraska Medical Center College of Medicine, University of New Mexico, University of North Carolina School of Medicine, University of Oklahoma College of Medicine, University of Oklahoma School of Community Medicine, Hospital of the University of Pennsylvania , University of Rochester Medical Center, USF Health, Morsani College of Medicine, University of Southern California Medical Center, University of Tennessee Medical Center, University of Texas Medical School, University of Texas Health, Sciences Center, University of Texas Medical Branch, University of Texas, Southwestern Medical School, University of Toledo, University of Utah Medical Center, University of Vermont College of Medicine, University of Virginia Health System, University of Washington, Medical Center, University of Wisconsin, Hospital & Clinics, University of Pittsburgh Medical Center, VA Caribbean Healthcare System, Vanderbilt University Medical Center, ECU Nephrology, Medical College of Virginia/Virginia Commonwealth University, Wake Forest School of Medicine, Washington Unviersity School of Medicine, West Virginia University, Winthrop University Hospital, Yale University School of Medicine, Div. Nephrology - RWTH Aachen University Hospital, Kazakh National Medical University, University of Pittsburgh School of Medicine, Kathmandu Medical College, All India Institute of Medical Science, Urology & Nephrology Center, Tabriz University of Medical Sciences,
Hacettepe University, Toronto General Hospital - University Health Network (UHN), Karolinska Institute, St Georges Healthcare NHS Trust, Gloucestershire Hospitals NHS Foundation Trust, University of Toronto - University Health Network - Toronto General Hospital, Northwestern University Medical School, Tulane University Medical School, Hedi Chaker Hospital - Department of Nephrology, Legacy Good Samaritan Hospital, Radbound University Nijmegen Medical Center, Hull & East Yorkshire
It's the delegate's responsibility to investigate the visa requirements for USA and to apply for a visa, if necessary. Individuals requiring an official Letter of Invitation from the conference organizers can request one by email by writing to us at kidney@nephroconferences.com
To receive a Letter of Invitation, delegates, accompanying persons/children, student/post-doc/youth delegates and exhibitors must first register for the conference.
The registration fee minus a handling fee of USD 100 will be refunded after the conference if the visa was applied for in time and proof is shown that a visa could not be granted even though all requested documents were submitted. Refund requests must be made in writing and sent to the Kidney 2018 via email.
All expenses incurred in relation to the conference are the sole responsibility of the delegate. The Letter of Invitation does not guarantee an entry visa to USA. However, the conference organizers will not directly contact embassies and consulates on behalf of delegates.
The deadline for requesting a Letter of Invitation is one month before travelling to USA.
Conference Highlights
- Kidney
- Acute Kidney Injury
- Chronic Kidney Disease
- Dialysis and Renal Care
- Kidney Transplantation
- Pediatric Nephrology
- Kidney Cancer
- Diabetic Kidney Disease
- Cardiovascular Impacts of Kidney Disease
- Glomerular-Tubulointerstitial Disorders
- Fluid, Electrolytes, Acid-Base Disorders
- CKD -Mineral and Bone Disorders
- Kidney and Bladder stones
- Urology/Urinary Tract Infections
- Geriatric-Genetic Kidney Diseases
- Renal Nutrition
- Nephrology Nursing
- Diagnosis of Kidney Diseases
- Renal Pathology-Immunology
- Drugs for Kidney Diseases
To share your views and research, please click here to register for the Conference.
To Collaborate Scientific Professionals around the World
| Conference Date | October 19-20, 2018 | ||
| Sponsors & Exhibitors |
|
||
| Speaker Opportunity Closed | Day 1 | Day 2 | |
| Poster Opportunity Closed | Click Here to View | ||
Useful Links
Special Issues
All accepted abstracts will be published in respective Our International Journals.
- Journal of Kidney
- Journal of Nephrology & Therapeutics
- Journal of Clinical & Experimental Nephrology
Abstracts will be provided with Digital Object Identifier by